Top Essay Writers
Our top essay writers are handpicked for their degree qualification, talent and freelance know-how. Each one brings deep expertise in their chosen subjects and a solid track record in academic writing.
Simply fill out the order form with your paper’s instructions in a few easy steps. This quick process ensures you’ll be matched with an expert writer who
Can meet your papers' specific grading rubric needs. Find the best write my essay assistance for your assignments- Affordable, plagiarism-free, and on time!
Posted: June 17th, 2024
Effect of glucocorticoids on serum level of omentin-1 and the possible link with insulin resistance in rats
Khaled Abdelfattah Abdelhamid Abulfadle
We get a lot of “Can you do MLA or APA?”—and yes, we can! Our writers ace every style—APA, MLA, Turabian, you name it. Tell us your preference, and we’ll format it flawlessly.
ABSTRACT
Background: Omentin-1 is an adipokine that decreases insulin resistance and its level is affected by body weight and serum adiponectin level changes, while, glucocorticoids are steroid hormones, secreted by adrenal cortex, affected insulin resistance, body weight and serum level of adiponectin.
Objective: This study was designed to investigate the possible effect of glucocorticoids on serum level of omentin-1 in male albino rats and the possible link with insulin resistance.
Design: 30 adult male albino rats, weighting 190-230 gm, were divided into three groups each of which included 10 rats; control, dexamethasone treated (Hyper-C) and metyrapone treated (Hypo-C). In (Hyper-C) group, rats were injected with dexamethasone (1mg/kg/day intra peritoneal) for two weeks. In (Hypo-C) group, metyrapone was administered orally dissolved in saline (200 mg/kg body weight) for two weeks. In the control group, normal saline was injected intraperitoneally (1 ml/rat/day) for two weeks. Rats were kept fasting for 8 hours and then, sacrificed under ether anesthesia by decapitation. Blood samples were collected and sera were separated and serum levels of omentin-1, corticosterone, ACTH, glucose and insulin were estimated. Insulin resistance (IR) was estimated by calculation of the homeostasis model assessment-IR (HOMA-IR) index. Body weights were measured at the start (initial body weight) of the study and just before rats being sacrificed (final body weight).
Totally! They’re a legit resource for sample papers to guide your work. Use them to learn structure, boost skills, and ace your grades—ethical and within the rules.
Results: There was a significant increase in body weight in Hyper-C group final weight (235.8±3.28), but, there was a significant decrease in body weight in Hypo-C group final weight (200±3.22) in comparison to that of control group final weight (217±2.85). On the other hand, there was a significant increase in serum levels of both glucose and insulin in Hyper-C group (237.8±10.4) and (4.88±0.16) in comparison to that in the control group (96.9±1.5) and (2.15±0.07) respectively. On the contrary, there was a significant decrease in serum levels of both glucose and insulin in Hypo-C group (72.2±2.2) and (1.28±0.1) in comparison to that in the Hyper-C group (237.8±10.4) and (4.88±0.16) respectively. Moreover, there was a significant decrease in HOMA-IR in the Hypo-C group (0.25±0.02) in comparison to that in the Hyper-C group (2.88±0.17). Furthermore, there was a significant decrease in serum omentin-1 level in Hyper-C group (14.5±0.47) but, a significant increase in its serum level in Hypo-C group (26.58±0.5) in comparison to that in the control group (21±0.35). On other hand, there were negative correlations in the Hyper-C group between serum omentin-1 and serum level of both insulin (R= -0.6, P Value= 0.07) and corticosterone (R= -0.22, P Value= 0.54), respectively.
Conclusion: The results of this study may explain a novel mechanism by which glucocorticoids cause insulin resistance and this is through the regulation of serum level of omentin-1. Also, the results confirmed presence of a link between serum levels of both glucocorticoids and omentin-1 which is mostly the change in body weight and this confirmed the importance of body weight control on glucose homeostasis.
Keywords: Omentin-1, Metyrapone, Dexamethasone, Glucose, Insulin resistance, ACTH, Corticosterone.
Starts at $10/page for undergrad, up to $21 for pro-level. Deadlines (3 hours to 14 days) and add-ons like VIP support adjust the cost. Discounts kick in at $500+—save more with big orders!
Introduction:
Omentin-1 is an adipocytokine, 35-kDa protein with 313 amino acids, that is expressed in visceral adipose tissue, endothelial cells, and, small intestine, and has insulin-sensitizing effects (Yang, Lee et al. 2006, Gürsoy, Kırnap et al. 2010, Chen, Shang et al. 2017). It has a preferred expression in visceral (omental) fat tissue (Yang, Xu et al. 2003). Two isoforms of Omentin are known, Omentin-1 and Omentin-2; Omentin-1 is the main circulating form (de Souza Batista, Yang et al. 2007, Zorlu, Kiskac et al. 2017). Omentin increased insulin-stimulated glucose uptake in human adipocytes in vitro and its expression in visceral adipose tissue is reduced in obesity and insulin resistance (Yang, Lee et al. 2006, de Souza Batista, Yang et al. 2007, Smitka and Maresova 2015). Brunetti, Orlando et al. (2013) stated that Omentin-1 has a central orexigenic function. Recently, Oswiecimska, Suwala et al. (2015) reported that serum omentin correlated negatively with serum insulin, and homeostasis model assessment-IR (HOMA-IR) index and they concluded that omentin is the nutritional marker reflecting body weight and insulin resistance. Herder, Ouwens et al. (2015) stated that omentin indirectly increased insulin sensitivity through adiponectin upregulation. On the other hand, Lee, Schnee et al. (2001) declared that excess of cortisol increases growth of visceral fat depots. Also, Morgan, Sherlock et al. (2009) stated that cortisol induced insulin resistance. Moreover, Purnell, Kahn et al. (2009) found that increased blood cortisol caused obesity and increased insulin resistance. Furthermore, Zhuang, Zhao et al. (2009) stated that although, visceral adipose tissue produced a large amount of omentin yet, its gene expression is reduced in visceral fat depot of obese subjects. Also, CÄ‚TOI, SUCIU et al. (2014) declared that omentin-1 enhanced adipocytes insulin-stimulated glucose uptake with no intrinsic insulin mimicking activity. Moreover, El€Mesallamy, El€Derany et al. (2011) stated that omentin level was decreased in overweight, impaired glucose regulation and diabetes type 2 patients. Furthermore, de Souza Batista, Yang et al. (2007) found that Omentin-1 plasma levels were positively correlated with the plasma adiponectin and inversely correlated with insulin resistance. Adiponectin is a known insulin-sensitizing adipokine (Kadowaki, Yamauchi et al. 2006) and its levels contribute to insulin resistance in obesity and type 2 diabetes mellitus (T2DM) while its high levels increase insulin sensitivity (Singh, Akhtar et al. 2012). Positive correlation of omentin-1 with adiponectin levels has been reported in patients with obesity and T2DM (de Souza Batista, Yang et al. 2007, Yan, Liu et al. 2011). On the other hand, glucocorticoids were found to decrease serum adiponectin level (Shi, Du et al. 2010). As glucocorticoids affect body weight, adiponectin level and insulin resistance, thus, the aim of this study was to evaluate the effect of changes in serum glucocorticoid, corticosterone, levels on serum omentin and to identify the possible link between glucocorticoids, omentin and insulin resistance and up to our knowledge there is no study confirmed this link.
Materials and methods:
Animals’ preparations and experimental protocol:
100%! We encrypt everything—your details stay secret. Papers are custom, original, and yours alone, so no one will ever know you used us.
30 adult male albino rats, weighting 190-230 gm, were purchased from the animal house of Zagazig University and were housed at 20-22°C on a 12-h light-dark cycle and for 5 days, to achieve acclimatization, they were supplied with tap water and a standard chow diet. Then, the rats were divided into three groups each of which included 10 rats; control, dexamethasone treated (Hyper-C) and metyrapone treated (Hypo-C). In (Hyper-C) group, rats were injected with dexamethasone (1mg/kg/day intra peritoneal) for two weeks (Burén, Lai et al. 2008). In (Hypo-C) group, metyrapone was used to induce hypocortism. It was administered orally dissolved in saline (200 mg/kg body weight) for two weeks (Miyamoto, Mitani et al. 1999). Adrenal cortex zona fasciculata cells contain glucocorticoid synthesizing enzyme, cytochrome P-45011ï¢, which is essential for synthesis of corticosterone in rats. Metyrapone, an inhibitor of the P-45011ï¢ï€ dependent l1ï¢-hydroxylase reaction was used to inhibit corticosterone synthesis (Miyamoto, Mitani et al. 1998). Metyrapone-treated rats were given 0.9% sodium chloride along with drinking water to compensate the loss of mineralocorticoids and thereby the ionic loss (Miyamoto, Mitani et al. 1999). In the control group, normal saline was injected intraperitoneally (1 ml/rat/day) for two weeks. Just after the end of the two weeks, the rats were kept fasting for 8 hours and then, sacrificed under ether anesthesia by decapitation.
Body weight changes among different groups:
Body weights of the used rats were measured in the different groups, initially at the start of the study (initial body weight) and finally at the end of the study just prior to being sacrificed by decapitation (final body weight).
Measurement of serum parameters:
Nope—all human, all the time. Our writers are pros with real degrees, crafting unique papers with expertise AI can’t replicate, checked for originality.
From all groups, blood samples were collected and sera were separated and stored at -20oC. An automated analyzer (YSI 2300; YSI Life Sciences, Yellow Springs, OH) was used to measure serum glucose through glucose oxidase method. Also, ELISA kits (R&D Systems, Minneapolis, MN) were used to estimate serum insulin. For evaluation of insulin resistance (IR), the homeostasis model assessment-IR (HOMA-IR) index was calculated by this equation:
HOMA-IR = 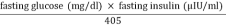 (Nayak, Hillemane et al. 2014).
(Nayak, Hillemane et al. 2014).
The index value is interpreted as follows: when the value of HOMA-IR increased, insulin resistance increased, which means decreased insulin sensitivity (Bonora, Targher et al. 2000). Thus, in order to know changes in insulin resistance among different groups, the value of the HOMA-IR index was compared among them. Serum omentin-1, ACTH and corticosterone levels were quantitated using commercially available ELISA kits as per manufacturer’s instructions (RayBiotech, Inc.; Catalog No. EIAR-OME), (Sigma-Aldrich, Catalog No. SE120080) and (Assaypro LLC, Catalog No. EC3001-1) respectively.
Statistical analysis:
Our writers are degree-holding pros who tackle any topic with skill. We ensure quality with top tools and offer revisions—perfect papers, even under pressure.
By the use of IBM SPSS Statistics for windows package version (24), data were analyzed and described as Mean± SEM. For calculation of the statistical significance, One-way ANOVA and Tukey HSD post hoc test for multiple group comparison were used. P‰¤0.05 indicated significance.
Results:
Table-1: Body weight (in gm) changes among different groups
|
Control Who Writes My Assignments?Experts with degrees—many rocking Master’s or higher—who’ve crushed our rigorous tests in their fields and academic writing. They’re student-savvy pros, ready to nail your essay with precision, blending teamwork with you to match your vision perfectly. Whether it’s a tricky topic or a tight deadline, they’ve got the skills to make it shine. |
Initial body weight |
205.5±2.64 |
|
Final body weight |
217±2.85a Will My Paper Be Unique?Guaranteed—100%! We write every piece from scratch—no AI, no copying—just fresh, well-researched work with proper citations, crafted by real experts. You can grab a plagiarism report to see it’s 95%+ original, giving you total peace of mind it’s one-of-a-kind and ready to impress. |
|
|
Hyper-C |
Initial body weight |
208.3±3.81a & c |
|
Final body weight Can You Use Any Citation Format?Yep—APA, Chicago, Harvard, MLA, Turabian, you name it! Our writers customize every detail to fit your assignment’s needs, ensuring it meets academic standards down to the last footnote or bibliography entry. They’re pros at making your paper look sharp and compliant, no matter the style guide. |
235.8±3.28b, d & e |
|
|
Hypo-C |
Initial body weight |
213±3.57a, c, f & g Can I Change My Order Details?For sure—you’re not locked in! Chat with your writer anytime through our handy system to update instructions, tweak the focus, or toss in new specifics, and they’ll adjust on the fly, even if they’re mid-draft. It’s all about keeping your paper exactly how you want it, hassle-free. |
|
Final body weight |
200±3.22a, d, f, g & h |
Data was expressed as Mean±SEM. a P>0.05 in comparison to the control group (initial body weight). b P<0.001 in comparison to the control group (initial body weight). c P>0.05 in comparison to the control group (final body weight). d P<0.01 in comparison to the control group (final body weight). e P<0.001 in comparison to the Hyper-C group (initial body weight). f P>0.05 in comparison to the Hyper-C group (initial body weight). g P<0.001 in comparison to the Hyper-C group (final body weight). h P>0.05 in comparison to the Hyper-C group (final body weight).
Table (1) showed changes in body weights of the used rats among different groups at the start (initial body weight) and just before rats being sacrificed (final body weight). In comparison to the control group initial body weight (205.5±2.64), there was a significant increase in body weight in the Hyper-C group finally (235.8±3.28), but, there were insignificant changes in body weight of the remaining groups. On the other hand, there was a significant increase in body weight in Hyper-C group final weight (235.8±3.28), but, there was a significant decrease in body weight in Hypo-C group final weight (200±3.22) in comparison to that of control group final weight (217±2.85). Also, there were insignificant changes in body weight in both Hyper-C group initial weight (208.3±3.81) and Hypo-C group initial weight (213±3.57) in comparison to that of control group final weight (217±2.85). Moreover, there was a significant increase in body weight in Hyper-C group final weight (235.8±3.28) in comparison to that of Hyper-C group initial weight (208.3±3.81), although, there were insignificant changes in body weight in both Hypo-C group initial weight (213±3.57) and Hypo-C group final weight (200±3.22) in comparison to that of Hyper-C group initial weight (208.3±3.81). Furthermore, there was a significant decrease in body weight in both Hypo-C group initial weight (213±3.57) and Hypo-C group final weight (200±3.22) in comparison to that of Hyper-C group final weight (235.8±3.28). Finally, there were insignificant changes in body weight in Hypo-C group final weight (200±3.22) in comparison to that of Hypo-C group initial weight (213±3.57). Table (2) showed changes in serum level of omentin-1, glucose, insulin, ACTH and corticosterone among different groups. Also, it showed changes in HOMA-IR among them. Regarding serum levels of corticosterone among different groups, there was a significant increase in its level in Hyper-C group (96.37±2.52), but a significant decrease in its level in Hypo-C group (8.08±0.32) in comparison to that in the control group (36.04±1.22). On the other hand, there was a significant decrease in serum level of corticosterone in Hypo-C group (8.08±0.32) in comparison to that in the Hyper-C group (96.37±2.52). On studying serum levels of ACTH, there was a significant decrease in its level in Hyper-C group (26.15±0.84), but a significant increase in its level in Hypo-C group (77.1±1.53) in comparison to that in the control group (46.75±1.2). On the other hand, there was a significant increase in serum level of ACTH in Hypo-C group (77.1±1.53) in comparison to that in the Hyper-C group (26.15±0.84). Regarding serum level of both glucose and insulin, there was a significant increase in serum level of both of them in Hyper-C group (237.8±10.4) and (4.88±0.16) in comparison to that in the control group (96.9±1.5) and (2.15±0.07) respectively. On the other hand, there was a significant decrease in serum level of both glucose and insulin in Hypo-C group (72.2±2.2) and (1.28±0.1) in comparison to that in the Hyper-C group (237.8±10.4) and (4.88±0.16) respectively. On other hand, on studying HOMA-IR among different groups, there was a significant increase in its value in Hyper-C group (2.88±0.17), but, there was an insignificant decrease in it in the Hypo-C group (0.25±0.02) in comparison to that in the control group (0.51±0.01). On the contrary, there was a significant decrease in HOMA-IR in the Hypo-C group (0.25±0.02) in comparison to that in the Hyper-C group (2.88±0.17). On studying serum omentin-1 level among different groups, there was a significant decrease in its serum level in Hyper-C group (14.5±0.47), but, there was a significant increase in its serum level in Hypo-C group (26.58±0.5) in comparison to the control group (21±0.35). Also, there was a significant increase in serum omentin-1 in Hypo-C group (26.58±0.5) in comparison to the Hyper-C group (14.5±0.47). Figure (1 A&B) showed negative correlations in the Hyper-C group between serum omentin-1 and both serum insulin (R= – 0.6, P Value= 0.07) and serum corticosterone (R= – 0.22, P Value= 0.54), respectively. On the other hand, figure (1 C&D) showed positive correlations in the Hypo-C group between serum omentin-1 and both serum insulin (R= 0.54, P Value= 0.11) and serum corticosterone (R= 0.6, P Value= 0.07), respectively.
It’s a breeze—submit your order online with a few clicks, then track progress with drafts as your writer brings it to life. Once it’s ready, download it from your account, review it, and release payment only when you’re totally satisfied—easy, affordable help whenever you need it. Plus, you can reach out to support 24/7 if you’ve got questions along the way!
Table-2: Serum omentin-1 (ng/ml), glucose (mg/dl), Insulin (ïIU/ml), HOMA-IR, ACTH (ng/ml), Corticosterone (nmol/L) among different groups:
|
Control |
Hyper-C |
Hypo-C How Quick Can You Write?Need it fast? We can whip up a top-quality paper in 24 hours—fully researched and polished, no corners cut. Just pick your deadline when you order, and we’ll hustle to make it happen, even for those nail-biting, last-minute turnarounds you didn’t see coming. |
|
|
Corticosterone (nmol/L) |
36.04±1.22 |
96.37±2.52a |
8.08±0.32a&b |
|
ACTH (ng/ml) Can You Handle Tough Topics?Absolutely—bring it on! Our writers, many with advanced degrees like Master’s or PhDs, thrive on challenges and dive deep into any subject, from obscure history to cutting-edge science. They’ll craft a standout paper with thorough research and clear writing, tailored to wow your professor. |
46.75±1.2 |
26.15±0.84a |
77.1±1.53a&b |
|
Glucose (mg/dl) |
96.9±1.5 How Do You Match Professor Expectations?We follow your rubric to a T—structure, evidence, tone. Editors refine it, ensuring it’s polished and ready to impress your prof. |
237.8±10.4a |
72.2±2.2b&c |
|
Insulin (ïIU/ml) |
2.15±0.07 How Do You Edit My Work?Send us your draft and goals—our editors enhance clarity, fix errors, and keep your style. You’ll get a pro-level paper fast. |
4.88±0.16a |
1.28±0.1a&b |
|
HOMA-IR |
0.51±0.01 |
2.88±0.17a Can You Brainstorm Topics?Yep! We’ll suggest ideas tailored to your field—engaging and manageable. Pick one, and we’ll build it into a killer paper. |
0.25±0.02b&d |
|
Omentin (ng/ml) |
21±0.35 |
14.5±0.47a |
26.58±0.5a&b |
Data was expressed as Mean±SEM. a P<0.001 in comparison to the control group. b P<0.001 in comparison to the Hyper-C group. c P<0.05 in comparison to the control group. d P>0.05 in comparison to the control group.
Figure-1: Correlations between; serum omentin-1 (ng/ml) and insulin (ïIU/ml) in Hyper-C group (A), serum omentin-1 (ng/ml) and corticosterone (nmol/l) in Hyper-C group (B), serum omentin-1 (ng/ml) and insulin (ïIU/ml) in Hypo-C group (C), serum omentin-1 (ng/ml) and corticosterone (nmol/l) in Hypo-C group (D). R, is the correlation coefficient. P Value, for the correlation, is considered significant when its value is ‰¤ 0.05.
Discussion:
The results of this study showed a significant increase in serum levels of corticosterone in Hyper-C group, but a significant decrease in its level in Hypo-C group in comparison to that in the control group. On the other hand, there was a significant decrease in serum levels of ACTH in Hyper-C group, but a significant increase in its level in Hypo-C group in comparison to that in the control group. These results were supported by Zardooz, Rostamkhani et al. (2010) who stated that increased serum levels of corticosterone were accompanied a significant decrease in serum levels of ACTH. Regarding serum glucose and insulin, the results of this study showed a significant increase in both of them in Hyper-C group in comparison to that in the control group. On the other hand, there was a significant decrease in serum glucose and insulin in Hypo-C group in comparison to that in the Hyper-C group. These results were supported by Morgan, Sherlock et al. (2009), Purnell, Kahn et al. (2009) and Zardooz, Rostamkhani et al. (2010) who found that increased serum levels of corticosterone significantly increased serum levels of both glucose and insulin as a result of increasing insulin resistance. Also, there was a significant increase in HOMA-IR in Hyper-C group, but, there was an insignificant decrease in it in the Hypo-C group in comparison to that in the control group. On the other hand, there was a significant decrease in HOMA-IR in the Hypo-C group in comparison to that in the Hyper-C group. These results reflects incidence of insulin resistance in Hyper-C group which was supported by Nanda, Mahapatra et al. (2015) who stated that insulin resistance is considered when the normal response of the tissues to insulin action is reduced, especially at the muscles and adipose tissues level with a compensatory hyperinsulinemia. Moreover, the results of this study showed a significant decrease in serum level of omentin-1 in Hyper-C group in comparison to the control group. This result confirmed that there is a link between omentin-1 and hyperglycemia as considered by Fu, Gong et al. (2004) who stated that, in the 1q22-q23 chromosomal region that was linked to type 2 diabetes mellitus, omentin gene was located. This was also supported by Yang, Lee et al. (2006), de Souza Batista, Yang et al. (2007), Tan, Adya et al. (2008), Yan, Liu et al. (2011), El€Mesallamy, El€Derany et al. (2011) and Shibata, Ouchi et al. (2012) and Nanda, Mahapatra et al. (2015) who found that increased serum glucose and insulin levels significantly decreased the serum level of omentin-1. This is further supported by Kazama, Usui et al. (2012), Oswiecimska, Suwala et al. (2015), Du, Ji et al. (2016) and Arman, Kirna et al. (2017) who stated that serum omentin-1 is correlated negatively with blood glucose, insulin and HOMA-IR. They explained this negative correlation by their results which declared that omentin-1 had adiponectin-like actions. On the other hand, the results of this study showed a significant increase in serum omentin-1 in Hypo-C group in comparison to that in both control and Hyper-C groups. This result was supported by Moreno-Navarrete, Catalán et al. (2010) and Saremi, Asghari et al. (2010) who found that omentin-1 serum level was increased by weight loss in obese patients. Also, the present study results declared a negative correlation between serum level of omentin-1 and that of both corticosterone and insulin in the Hyper-C group. These results confirmed that there was a negative relationship between serum omentin-1 level and insulin resistance which was supported by de Souza Batista, Yang et al. (2007) and Tan, Adya et al. (2008) who found that serum level of omentin-1 was correlated negatively with insulin resistance and they explained this relation by the positive correlation between serum level of omentin-1 and that of adiponectin. This is also was supported by Yang, Lee et al. (2006), Gürsoy, Kırnap et al. (2010), CÄ‚TOI, SUCIU et al. (2014), Herder, Ouwens et al. (2015) and Chen, Shang et al. (2017) who found that, in adipose tissue, omentin has an insulin sensitizing action through increasing both insulin signal transduction and insulin effects by stimulating glucose uptake in an insulin-mediated manner. Moreover, Herder, Ouwens et al. (2015) stated that omentin indirectly increased insulin sensitivity through adiponectin upregulation. Furthermore, Cai, Wei et al. (2009), Pan, Guo et al. (2010) and Nanda, Mahapatra et al. (2015) supported the incidence of insulin resistance with the decrease in serum omentin-1 levels as they found that in insulin resistance diabetic patients, the serum insulin level and HOMA-IR score were high while, serum omentin-1 level was low. On the other hand, the results of this study showed a significant increase in the final body weight in the Hyper-C group, but, a significant decrease in the final body weight in the Hypo-C group in comparison to that in the control group final body weight. These results were accompanied, as mentioned early, by a significant decrease in serum omentin-1 level in Hyper-C group, but a significant increase in its level in Hypo-C group in comparison to that in the control group. These finding were supported by Lee, Schnee et al. (2001) and Purnell, Kahn et al. (2009) who stated that excess of glucocorticoids significantly increased body weight. Also, Zhuang, Zhao et al. (2009), Xu, Huang et al. (2010), El€Mesallamy, El€Derany et al. (2011) and Feng, Yuan et al. (2013) reported reduction in serum omentin-1 level with the increase in body weight. The significant changes in the final body weights in the Hyper-C and Hypo-C groups in comparison to the control group in the results of this study, may explain the possible link between glucocorticoids, omentin-1 and insulin resistance as corticosterone levels significantly affected final body weight which in turn affected serum level of omentin-1 and insulin resistance. These results were supported by Yang, Lee et al. (2006), de Souza Batista, Yang et al. (2007), Oswiecimska, Suwala et al. (2015) and Smitka and Maresova (2015) who stated that omentin expression in visceral adipose tissue is reduced in obesity and insulin resistance. Also, Oswiecimska, Suwala et al. (2015) considered omentin as a nutritional marker that reflected the body weight. From the above discussed results, it was clear that glucocorticoids may be one of the regulators for omentin-1 and changes in body weight accompanied the abnormal serum levels of glucocorticoids may explain that regulation. This may also give a new explanation for the changes in insulin resistance that occur with abnormal serum levels of glucocorticoids. Also, it confirmed the importance of body weight control on glucose homeostasis.
Conclusion
The results of this study may explain a novel mechanism by which glucocorticoids cause insulin resistance and this possibly through the regulation of serum level of omentin-1. Also, the results confirmed presence of a link between serum levels of both glucocorticoids and omentin-1 which is mostly the change in body weight and this confirmed the importance of body weight control on glucose homeostasis. Further studied should be conducted to confirm these results.
Tags: 1500 Words Assessment Task, Ace Homework Tutors, Assignment Homework Help & Answers, Bishops Writing BureauYou Want The Best Grades and That’s What We Deliver
Our top essay writers are handpicked for their degree qualification, talent and freelance know-how. Each one brings deep expertise in their chosen subjects and a solid track record in academic writing.
We offer the lowest possible pricing for each research paper while still providing the best writers;no compromise on quality. Our costs are fair and reasonable to college students compared to other custom writing services.
You’ll never get a paper from us with plagiarism or that robotic AI feel. We carefully research, write, cite and check every final draft before sending it your way.